Distinct Mutations in Calcium Channel Gene May Lead to LGS, Study Suggests
Written by |
Distinct mutations in the CACNA1A gene — which contains instructions for producing a subunit of CaV2.1, a calcium channel key to nerve cell communication — are associated with Lennox-Gastaut syndrome (LGS), a study suggests.
Assessing the impact of these different CACNA1A mutations in CaV2.1’s function and location may help to develop and determine appropriate therapies for this patient population, the researchers said.
The study, “Both gain‐of‐function and loss‐of‐function de novo CACNA1A mutations cause severe developmental epileptic encephalopathies in the spectrum of Lennox‐Gastaut syndrome,” was published in the journal Epilepsia.
LGS belongs to a group of rare early-onset epileptic disorders called developmental and epileptic encephalopathies, or DEEs, which are characterized by treatment-resistant seizures, developmental delays, cognitive and behavioral problems, and changes in the brain’s electric activity.
While a large proportion of DEEs results from brain malformations and brain lesions occurring before or right after birth, a genetic cause has been identified in around 35–40% of people with this disease. Most DEE-associated mutations are sporadic, called de novo, rather than inherited, meaning that they appear for the first time in one family member.
Scientists have found an association between inherited loss-of-function mutations in the CACNA1A gene — meaning that these alterations result in the production of less, or of a non-functional subunit of CaV2.1 — and the development of DEEs.
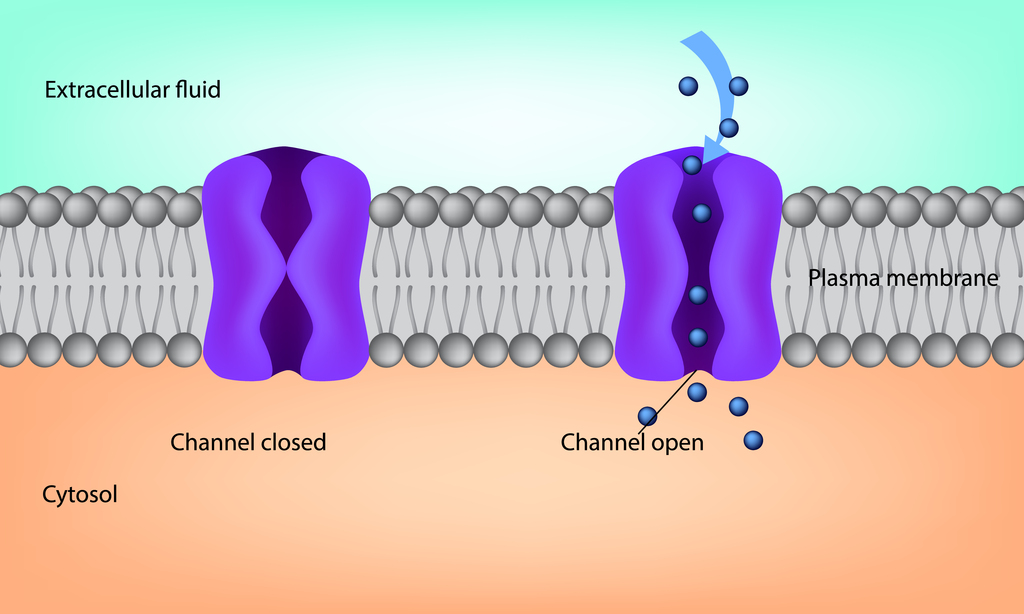
Cav2.1, present on the membrane of nerve cells, is the major channel responsible for fast signal transmission between nerve cells.
Moreover, de novo CACNA1A missense mutations have been identified in 1% of children with more severe DEE in the spectrum of Lennox-Gastaut syndrome. Missense mutations are aberrations in single nucleotides — the building blocks of proteins — that alter protein composition.
“Thus de novo CACNA1A variants may be an important and recurrent cause of severe neurodevelopmental disorders,” the researchers said.
However, how these de novo mutations cause DEEs, including LGS, remains unclear.
To learn more, the researchers now set out to evaluate the functional impact of four de novo CACNA1A missense mutations identified in four children with LGS-associated symptoms.
All of the children — two boys and two girls — presented with different types of seizures, global developmental delay, moderate-to-severe intellectual disability, impaired movement coordination, and abnormalities in the brain’s electric activity. Treatment-resistant seizures began in early infancy, between the ages of 2 days and 6 months.
While one of the mutations — p.A713T — had been previously reported, the other three — p.V1396M, p.G230V, and p.I1357S — were identified for the first time. All were considered disease-causative by two validated informatic systems.
The researchers analyzed the effects of these aberrations on CaV2.1’s function and location in human cells and in mouse nerve cells grown in the lab. Their resulting structural changes were predicted using informatic three-dimensional programs.
The results showed that the G230V and I1357S mutations impaired CaV2.1’s function and reduced its transport to the cell membrane, with fewer channels detected at that location. These were loss‐of‐function effects.
By contrast, A713T and V1396M mutations resulted in a higher-than-normal CaV2.1 function, facilitating the channel’s voltage-dependent activation for gain-of-function effects. In addition, informatic analysis predicted that both alterations caused protein structural changes favoring channel opening, and thus, more activation.
“We provide functional evidence demonstrating that these DEE‐associated CACNA1A de novo mutations indeed alter CaV2.1 channel function through either a gain‐of‐function or a loss‐of‐ function effect,” the researchers said.
The team noted that both CACNA1A loss-of-function and gain-of-function mutations can result in similar epileptic conditions. This may be due to the mutations’ distinct and divergent impact on different components of the nerve cell circuits.
“Clarifying the mechanisms by which specific mutations affect the function and localization of CaV2.1 channels will improve therapeutic interventions for patients with CACNA1A‐associated DEEs,” the researchers said.
The team hypothesized that children carrying CACNA1A loss-of-function mutations might respond to treatments designed to boost CaV2.1 transport to the cell membrane. Meanwhile, children with gain-of-function alterations might respond to treatments blocking CaV2.1, they said.
The researchers also emphasized that the clinical characterization of more patients with CACNA1A missense mutations and DEEs, along with the assessment of the functional impact of these alterations, may help distinguish symptoms associated with CACNA1A loss- and gain-of function mutations.